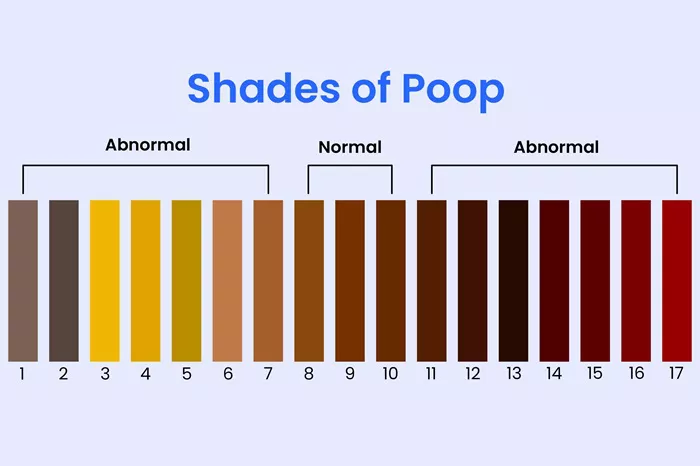
When jaundice sets in, the body’s normal processes of bilirubin metabolism are disrupted, and this disruption reverberates through various outward signs, one of the most notable being alterations in the color of feces. Parents, caregivers, and even individuals themselves need to be attuned to these changes as they can provide valuable insights into the severity and nature of the jaundice, guiding appropriate medical action. The color of poop during jaundice is not a random occurrence but a direct reflection of what’s happening within the complex machinery of the liver, bile ducts, and intestines as they grapple with the abnormal levels of bilirubin.
The Physiology of Normal Stool Color and the Entry of Jaundice
Under normal circumstances, bile, which is produced by the liver and stored in the gallbladder, plays a pivotal role in determining stool color. Bile contains bilirubin, which has been conjugated (chemically modified to be water-soluble) by the liver. When food moves through the digestive tract, bile is released into the small intestine to aid in the emulsification and digestion of fats. As the bilirubin in bile travels through the intestines, it undergoes further chemical changes due to the action of bacteria. The end result is the characteristic brown color of healthy stools. However, in jaundice, the story takes a different turn. The liver’s ability to properly process and excrete bilirubin is hampered, leading to an accumulation of bilirubin in the body. This excess bilirubin then finds its way into the digestive system, but not in the usual, well-regulated manner, causing distinct changes in stool appearance.
Neonatal Jaundice and Stool Color
1. Physiological Neonatal Jaundice: Subtle Shifts
In the case of physiological neonatal jaundice, which is relatively common in the first few days after birth due to the liver’s immaturity, the stool color might initially show only mild alterations. Newborns with this mild form of jaundice often have stools that are slightly paler than the normal rich brown. The liver is still learning to efficiently handle bilirubin, and while it manages to secrete some bile with conjugated bilirubin into the intestines, the quantity and quality might not be at the optimal level. Parents may notice that the diaper contents are more of a tan or light brown shade rather than the deep, earthy brown seen in healthy infants. This is a sign that the bilirubin metabolism is a bit sluggish but usually resolves on its own as the liver matures over the course of the first week or two of life.
2. Pathological Neonatal Jaundice: More Drastic Changes
When neonatal jaundice is due to pathological causes such as blood group incompatibilities (like ABO or Rh incompatibilities between mother and baby), infections, or congenital enzyme deficiencies, the stool color changes can be more pronounced. In cases of severe hemolytic jaundice caused by blood group issues, the stools can become extremely pale, almost white or a very light gray. This is because the rapid destruction of red blood cells leads to a massive influx of bilirubin that the liver struggles to process and conjugate effectively. Without proper conjugation, the bilirubin doesn’t get incorporated into the bile in the right way, and as a result, there’s a lack of the normal pigment that gives stools their color.
Additionally, if there’s an obstruction in the bile ducts, perhaps due to a congenital anomaly like biliary atresia, bile flow to the intestines is severely restricted or completely blocked. This also leads to stools that are achromatic, resembling clay in appearance, as no bile reaches the digestive tract to impart color. These pale stools are often accompanied by other symptoms like dark urine (as the body tries to excrete the unprocessed bilirubin through the kidneys) and a more intense yellowing of the skin and eyes, flagging the need for urgent medical evaluation and intervention.
Jaundice in Children and Adolescents: Varied Color Manifestations
1. Infectious Jaundice: From Dark to Pale
When children or adolescents develop jaundice due to infectious agents like viral hepatitis (hepatitis A, B, C, etc.), the stool color can change depending on the stage and severity of the infection. In the early stages of hepatitis, the liver inflammation might cause a backup of bile within the liver, and as a result, less bile is released into the intestines. This can lead to stools that start to turn paler, losing their usual brown hue. As the infection progresses and the liver’s function becomes more compromised, the stool color can become a very light yellowish-brown or even approach a whitish-gray shade, similar to what’s seen in severe neonatal pathological jaundice. The change in color is often accompanied by other symptoms such as abdominal pain, nausea, vomiting, fatigue, and of course, the yellowing of the skin and eyes. Monitoring stool color along with these symptoms helps parents and healthcare providers gauge the effectiveness of treatment and the recovery of liver function.
2. Metabolic and Genetic Disorders: Unusual Tints
In cases of metabolic or genetic disorders that lead to jaundice, like Gilbert’s syndrome or Crigler-Najjar syndrome, the stool color might exhibit unique patterns. Gilbert’s syndrome, which is a relatively mild genetic condition affecting bilirubin conjugation, can cause intermittent jaundice. During these episodes, the stool color may be slightly paler than normal, with a more yellowish undertone compared to the typical brown. This is because the fluctuating levels of unconjugated bilirubin in the body affect the amount and quality of bile that reaches the intestines. In Crigler-Najjar syndrome, which is much more severe and involves a significant defect in bilirubin conjugation, the stools can be persistently pale, almost white, as the liver is unable to properly process and excrete bilirubin, leading to a lack of the normal pigmentation in the feces, much like in some of the more serious obstructive jaundice cases.
Adult Jaundice and Stool Alterations
1. Lifestyle-Related and Viral-Induced Jaundice: Progressive Changes
In adults, jaundice can stem from lifestyle factors such as chronic alcohol abuse or viral infections. In the case of chronic alcohol-induced liver damage (alcoholic hepatitis or cirrhosis), the liver’s ability to produce and secrete bile deteriorates over time. Initially, the stool color might become a bit lighter, with a duller brown shade, as the liver struggles to maintain normal bile flow. As the condition worsens, the stools can turn a pale yellowish-gray, indicating that the liver is severely compromised in its function of getting bile into the digestive tract. With viral hepatitis in adults, similar to the pediatric scenario, the stool color changes in tandem with the progression of the liver inflammation and impairment of bile secretion, starting from a mild paleness and potentially progressing to a more significant loss of color, depending on the effectiveness of treatment and the body’s ability to fight off the virus.
2. Obstructive Jaundice: The Clay-Like Appearance
When adults develop obstructive jaundice, perhaps due to gallstones lodged in the bile ducts, tumors in the liver, pancreas, or bile ducts, the stool color takes on a very distinct and concerning appearance. The stools become a chalky, clay-like white or very light gray color. This is because the physical blockage in the bile ducts completely or almost completely halts the flow of bile to the intestines. Without bile reaching the digestive tract, there’s no pigment to give the stools their normal brown color. This drastic change in stool color, along with the associated symptoms of jaundice like yellow skin and eyes, itchy skin (due to the buildup of bile salts in the body), and abdominal pain (especially if caused by a gallstone or tumor), signals the need for immediate medical attention to identify and address the underlying cause of the obstruction.
Conclusion
The color of poop during jaundice serves as a vital indicator of the inner workings of the body’s bilirubin management system. From the subtle paleness in mild neonatal jaundice to the extreme white or clay-like stools in severe obstructive cases, these color changes tell a story of liver function, bile flow, and the body’s struggle to handle abnormal levels of bilirubin. Parents, caregivers, and individuals should be vigilant about observing stool color, especially when jaundice is suspected or diagnosed, as it can provide early warnings, guide medical decisions, and help in tracking the progress of treatment and recovery. Understanding the nuances of jaundice-related stool color is an essential piece of the puzzle in ensuring the well-being of those affected by this condition, whether they are the tiniest newborns or adults dealing with complex health issues. By paying close attention to this seemingly simple yet highly informative sign, we can take proactive steps in the journey to manage and overcome jaundice.
Related Topics: