Jaundice, characterized by the yellowing of the skin and eyes, is a common condition in newborns. It occurs due to the accumulation of bilirubin, a yellow pigment produced during the normal breakdown of red blood cells. While mild jaundice often resolves on its own, more severe cases require medical intervention to prevent serious complications. One of the most effective treatments for neonatal jaundice is phototherapy. This article explores why phototherapy is used for jaundice, how it works, its benefits, and what to expect during treatment.
Understanding Neonatal Jaundice
What is Jaundice?
Jaundice is a condition that causes yellowing of the skin, eyes, and mucous membranes due to high levels of bilirubin in the blood. In newborns, this is often called neonatal jaundice. Bilirubin is a byproduct of the normal breakdown of red blood cells. The liver processes bilirubin, which is then excreted from the body. However, in newborns, the liver may not be fully developed, leading to a temporary buildup of bilirubin.
Causes of Neonatal Jaundice
Several factors can contribute to the development of jaundice in newborns:
Physiological Jaundice: Most common, occurring in almost all newborns to some extent. It usually appears between the second and fourth day of life and resolves within one to two weeks.
Breastfeeding Jaundice: Linked to inadequate milk intake in the first few days of life, leading to dehydration and decreased bilirubin excretion.
Breast Milk Jaundice: Occurs after the first week of life and is thought to be related to substances in breast milk that inhibit bilirubin excretion.
Hemolytic Jaundice: Caused by blood group incompatibility between mother and baby, leading to increased red blood cell breakdown.
Prematurity: Preterm infants have underdeveloped livers, which makes it more challenging to process bilirubin.
The Need for Phototherapy
When is Phototherapy Recommended?
Phototherapy is recommended for newborns with elevated bilirubin levels that pose a risk for bilirubin-induced neurological dysfunction (BIND) or kernicterus, a form of brain damage caused by excessive bilirubin. The decision to start phototherapy depends on several factors, including the baby’s age, bilirubin levels, and overall health.
Risks of Untreated Jaundice
If left untreated, high bilirubin levels can lead to severe complications:
Kernicterus: This is the most severe form of bilirubin toxicity, leading to permanent brain damage, hearing loss, vision problems, and intellectual disabilities.
Acute Bilirubin Encephalopathy: Early signs include lethargy, poor feeding, and high-pitched crying. If not treated promptly, it can progress to seizures and coma.
How Phototherapy Works
The Science Behind Phototherapy
Phototherapy involves exposing the baby’s skin to a specific wavelength of light, typically in the blue spectrum (around 460-490 nm). This light transforms bilirubin into a water-soluble form that can be excreted through the baby’s urine and stool without needing further processing by the liver.
Types of Phototherapy
There are several types of phototherapy, including:
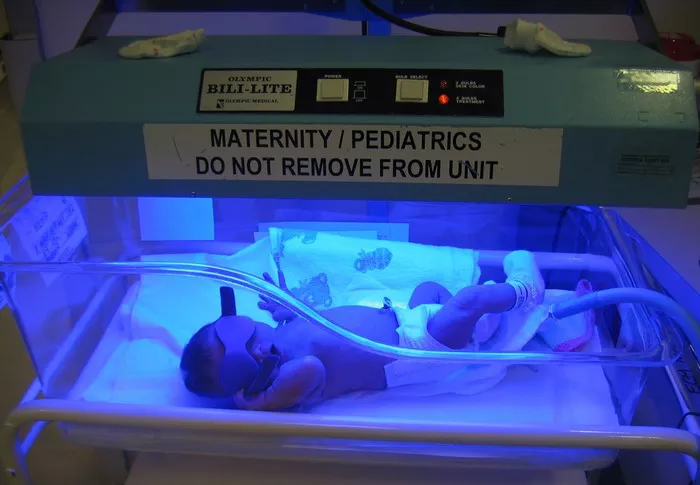
Conventional Phototherapy: Uses fluorescent or LED lights placed over the baby, who lies in an incubator or bassinet.
Fiberoptic Phototherapy: Involves a light-emitting pad or blanket that wraps around the baby, allowing for more direct and comfortable treatment.
Intensive Phototherapy: Combines multiple light sources and wavelengths for more effective treatment, often used in severe cases.
Treatment Duration and Monitoring
The duration of phototherapy varies depending on the baby’s bilirubin levels and response to treatment. Continuous monitoring of bilirubin levels is essential to determine the effectiveness of phototherapy and decide when to stop treatment.
Benefits of Phototherapy
Rapid Reduction of Bilirubin Levels
Phototherapy is highly effective in rapidly lowering bilirubin levels, often within 24 to 48 hours. This swift action is crucial in preventing the harmful effects of high bilirubin levels.
Non-Invasive and Painless
One of the significant advantages of phototherapy is that it is non-invasive and painless. Babies usually tolerate the treatment well, and it can be administered in a hospital setting or at home under medical supervision.
Safety and Efficacy
Phototherapy is a well-established and safe treatment for neonatal jaundice. When administered correctly, it poses minimal risks and has a high success rate in reducing bilirubin levels to safe ranges.
Flexibility in Administration
With advancements in technology, phototherapy can be tailored to the needs of each baby. Fiberoptic blankets allow for continuous treatment even when the baby is being held or fed, providing flexibility and convenience for parents and caregivers.
See Also: What Are the Dangers of Jaundice in Newborns?
What to Expect During Phototherapy
Preparation for Phototherapy
Before starting phototherapy, healthcare providers will explain the procedure and its benefits to the parents. The baby’s eyes will be covered with protective shields to prevent potential damage from the light exposure.
During the Treatment
The baby will be placed under the phototherapy lights, either in an incubator or a bassinet, wearing only a diaper to maximize skin exposure. It is essential to ensure that the baby remains adequately hydrated, as phototherapy can increase fluid loss.
Monitoring and Adjustments
Regular monitoring of bilirubin levels, body temperature, and hydration status is crucial during phototherapy. Healthcare providers may adjust the light intensity or the type of phototherapy based on the baby’s response to treatment.
Post-Phototherapy Care
Once bilirubin levels reach a safe range, phototherapy can be discontinued. The baby’s bilirubin levels will continue to be monitored to ensure they do not rise again. Parents will receive instructions on what to watch for and when to seek further medical advice.
Potential Side Effects of Phototherapy
While phototherapy is generally safe, it is essential to be aware of potential side effects, including:
Dehydration: Increased fluid loss can occur, so close monitoring of hydration status is necessary.
Temperature Instability: Babies may experience fluctuations in body temperature, requiring careful monitoring.
Skin Rash: Some babies may develop a mild skin rash, which typically resolves after treatment.
Loose Stools: Increased bilirubin excretion can lead to more frequent and loose stools.
Conclusion
Phototherapy is a critical and effective treatment for neonatal jaundice. By rapidly reducing bilirubin levels, it prevents the severe complications associated with high bilirubin, such as kernicterus and acute bilirubin encephalopathy. Its non-invasive, painless nature and high success rate make it the preferred treatment option for managing jaundice in newborns. Understanding the importance of phototherapy, how it works, and what to expect during treatment can help parents and caregivers feel more confident and prepared when their newborn requires this lifesaving intervention.