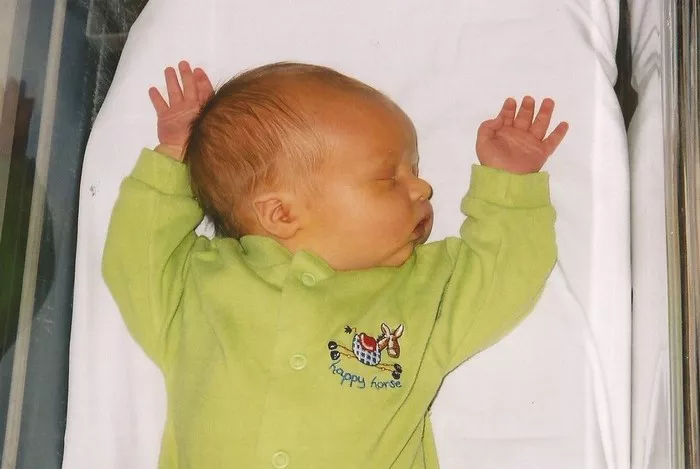
Jaundice is a common condition in newborns that results from elevated levels of bilirubin in the blood, causing yellowing of the skin and eyes. While often harmless, severe cases can lead to serious complications. It is crucial for parents and caregivers to recognize the signs, understand the risk factors, and be aware of the potential dangers associated with neonatal jaundice.
Introduction to Neonatal Jaundice
Neonatal jaundice, characterized by the yellow discoloration of the skin and sclerae (whites of the eyes), affects a significant number of newborns worldwide. It occurs due to the accumulation of bilirubin, a yellow pigment produced from the breakdown of red blood cells. In most cases, jaundice appears within the first week of life and typically resolves on its own without intervention. However, certain factors can increase the risk of severe jaundice, which necessitates medical attention to prevent complications.
Causes and Risk Factors
Understanding the causes and risk factors of neonatal jaundice is essential for early identification and management. The most common reasons include:
1. Physiological Jaundice: This is the most frequent type of jaundice in newborns, occurring as a result of the immature liver’s inability to efficiently process bilirubin.
2. Breastfeeding Jaundice: Inadequate intake of breast milk can lead to dehydration and reduced bilirubin elimination, contributing to jaundice.
3. Blood Group Incompatibility: Rh or ABO blood group incompatibility between the mother and the baby can cause increased breakdown of red blood cells and subsequent bilirubin production.
4. Enzyme Deficiencies: Certain genetic conditions, such as glucose-6-phosphate dehydrogenase (G6PD) deficiency, can predispose newborns to jaundice.
5. Prematurity: Preterm infants are at higher risk due to their underdeveloped liver function and higher red blood cell turnover.
Identifying these factors can help healthcare providers assess the likelihood of severe jaundice and implement appropriate monitoring and treatment measures.
Complications of Severe Jaundice
While most cases of neonatal jaundice resolve without intervention, severe or untreated jaundice can lead to serious complications:
1. Acute Bilirubin Encephalopathy: This occurs when high levels of bilirubin cross the blood-brain barrier and deposit in the brain tissue, leading to neurological damage. Symptoms include lethargy, poor feeding, high-pitched crying, and abnormal muscle tone.
2. Kernicterus: Kernicterus is a rare but devastating condition characterized by irreversible damage to the brain due to severe jaundice. It can cause cerebral palsy, hearing loss, intellectual disabilities, and even death.
3. Long-Term Neurodevelopmental Impairments: Even without reaching the level of kernicterus, prolonged exposure to high bilirubin levels can impair neurodevelopmental outcomes, leading to learning disabilities, behavioral problems, and poor academic performance later in life.
Diagnosis and Monitoring
Early diagnosis and monitoring of jaundice are crucial to prevent complications. Healthcare providers typically assess jaundice using a combination of clinical observation and bilirubin level measurements. Techniques such as transcutaneous bilirubinometry and serum bilirubin testing help determine the severity of jaundice and guide treatment decisions.
Management and Treatment Options
Management strategies for neonatal jaundice depend on the underlying cause and severity:
1. Phototherapy: Phototherapy involves exposing the baby’s skin to special blue lights that help break down bilirubin into a form that the body can more easily eliminate.
See Also: When Does Jaundice Appear in Newborns: Things You Need to Know
2. Exchange Transfusion: In severe cases where phototherapy is ineffective or when bilirubin levels are dangerously high, exchange transfusion may be necessary. This procedure involves gradually replacing the baby’s blood with donor blood to reduce bilirubin levels.
3. Addressing Underlying Causes: Treating underlying conditions such as infections or blood group incompatibilities that contribute to jaundice is essential in managing the condition.
Prevention Strategies
While not all cases of neonatal jaundice can be prevented, there are steps parents and healthcare providers can take to reduce the risk of severe jaundice:
1. Early and Regular Feeding: Ensuring adequate intake of breast milk or formula can promote regular bowel movements and eliminate bilirubin from the body.
2. Monitoring Bilirubin Levels: Regular monitoring of bilirubin levels in at-risk infants allows for early intervention if levels begin to rise.
3. Educating Parents: Providing education on the signs of jaundice and when to seek medical attention empowers parents to recognize potential issues early.
Conclusion
Neonatal jaundice is a common condition that affects many newborns worldwide. While often benign, severe cases can lead to significant neurological complications if left untreated. Early recognition, monitoring, and appropriate management are essential in preventing adverse outcomes associated with severe jaundice. By understanding the causes, risk factors, and potential complications of neonatal jaundice, healthcare providers and parents can work together to ensure optimal outcomes for newborns affected by this condition. Vigilance and prompt medical intervention are key in mitigating the dangers posed by neonatal jaundice and promoting the health and well-being of infants everywhere.