Jaundice, characterized by the yellowing of the skin and the whites of the eyes, is a condition that can affect individuals of all ages, including adults. It often signals an underlying issue with bilirubin metabolism, which could stem from various causes such as liver diseases, gallbladder problems, or blood disorders. Vitamin D, on the other hand, is a crucial nutrient known for its role in bone health, immune function, and numerous other physiological processes. The question of whether vitamin D can play a beneficial role in managing jaundice in adults has piqued the interest of both medical professionals and patients alike. In this article, we will explore the relationship between vitamin D and adult jaundice in-depth, examining the current scientific evidence, potential mechanisms of action, and implications for treatment.
Understanding Jaundice in Adults
1. Causes of Adult Jaundice
Adult jaundice can arise from multiple sources. Liver diseases like hepatitis (viral, autoimmune, or drug-induced), cirrhosis (resulting from chronic liver damage due to alcohol abuse, hepatitis, or other factors), and liver cancer can disrupt the normal processing and excretion of bilirubin. Gallbladder and biliary tract issues, such as gallstones that block the bile ducts or inflammation of the bile ducts (cholangitis), impede the flow of bile containing conjugated bilirubin into the intestines, leading to its backup and subsequent jaundice. Additionally, certain blood disorders, including hemolytic anemias where red blood cells are prematurely destroyed, generate an excessive amount of bilirubin that the liver struggles to handle efficiently.
2. Diagnosis and Clinical Presentation
Diagnosing jaundice in adults typically begins with a physical examination, where the doctor notes the yellowish discoloration of the skin and sclera. Laboratory tests play a crucial role, measuring total bilirubin, conjugated (direct) bilirubin, and unconjugated (indirect) bilirubin levels in the blood. Imaging studies like ultrasounds, CT scans, or MRIs may be ordered to visualize the liver, gallbladder, and biliary tract for potential structural abnormalities. Clinically, patients may experience symptoms beyond the visible yellowing, such as fatigue, abdominal pain (especially in the right upper quadrant where the liver and gallbladder are located), itching due to the deposition of bilirubin in the skin, and changes in urine and stool color (dark urine and pale stools).
The Role of Vitamin D in the Body
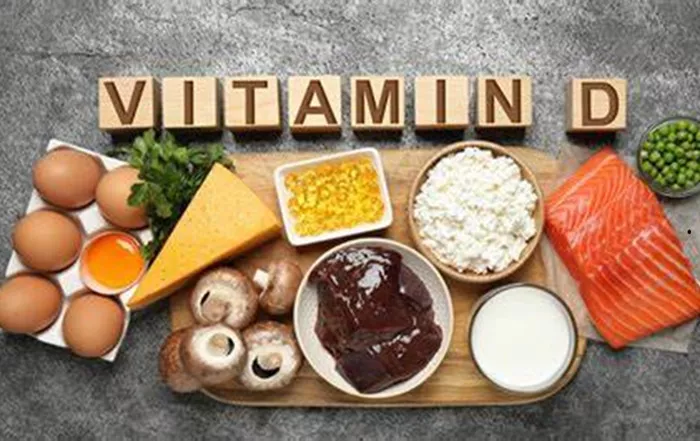
1. Vitamin D Sources and Metabolism
Vitamin D can be obtained through two primary sources: sunlight exposure and dietary intake. When the skin is exposed to ultraviolet B (UVB) rays from the sun, a precursor molecule in the skin is converted into previtamin D3, which then undergoes further modifications in the liver and kidneys to become the active form, 1,25-dihydroxyvitamin D (calcitriol). Dietary sources include fatty fish (such as salmon, mackerel, and tuna), fortified dairy products, and supplements. Vitamin D receptors are widespread throughout the body, found in tissues like the bones, intestines, kidneys, and immune cells, highlighting its pleiotropic effects on various physiological functions.
2. Established Health Benefits
Traditionally, vitamin D is renowned for its role in calcium homeostasis and bone health. It promotes calcium absorption in the intestines, aids in bone mineralization, and helps regulate bone remodeling, reducing the risk of conditions like osteoporosis and rickets. Beyond bone health, emerging research has shown its involvement in modulating the immune system, with potential implications for autoimmune diseases, infectious diseases, and even cancer prevention. It also plays a role in muscle function, cardiovascular health, and cognitive function, although the exact mechanisms in these areas are still being elucidated.
The Link between Vitamin D and Jaundice in Adults: Scientific Evidence
1. In Vitro and Animal Studies
Some in vitro studies have explored the relationship between vitamin D and bilirubin metabolism at the cellular level. Research on liver cells in culture has suggested that vitamin D may influence the expression of genes involved in bilirubin conjugation and excretion. In animal models of liver disease and jaundice, supplementation with vitamin D has shown promising results in reducing bilirubin levels, improving liver function markers, and mitigating liver damage. For example, in a mouse model of hepatitis-induced jaundice, animals given vitamin D supplements had better outcomes in terms of reduced jaundice severity and improved liver histology compared to control animals. However, it’s important to note that animal models may not perfectly replicate human physiology and pathology, and further translation to human studies is needed.
2. Human Clinical Studies
In human clinical trials, the evidence regarding vitamin D’s efficacy in treating jaundice in adults is less conclusive. Some small-scale studies have investigated the impact of vitamin D supplementation on jaundice in patients with liver cirrhosis or hepatitis. While a few have reported a modest reduction in bilirubin levels and improved symptoms such as fatigue and itching in the supplemented group compared to placebo, others have found no significant difference. Larger, well-designed randomized controlled trials (RCTs) are lacking, which makes it difficult to draw definitive conclusions about the true therapeutic value of vitamin D in adult jaundice. Additionally, many of the existing studies have limitations in terms of sample size, heterogeneity of patient populations (with different underlying causes of jaundice), and the duration and dosage of vitamin D supplementation used.
Potential Mechanisms of Action
1. Modulation of Liver Function
Vitamin D may act on liver cells by binding to its receptors present in the liver tissue. This binding could potentially upregulate the expression of enzymes involved in bilirubin conjugation, such as glucuronyl transferase, which is crucial for making bilirubin water-soluble and facilitating its excretion through bile. By enhancing the liver’s capacity to process bilirubin, vitamin D could help reduce the buildup of bilirubin in the body and alleviate jaundice symptoms.
2. Anti-Inflammatory and Immunomodulatory Effects
In cases where jaundice is caused by inflammatory liver diseases or autoimmune disorders, vitamin D’s anti-inflammatory and immunomodulatory properties may come into play. It can suppress the activation of immune cells, such as macrophages and T cells, that contribute to liver inflammation. By reducing inflammation in the liver, the normal function of liver cells can be better preserved, allowing for more efficient bilirubin metabolism and clearance.
3. Support for Biliary Tract Health
There is also speculation that vitamin D could have a beneficial effect on the biliary tract. It may help maintain the integrity of the bile ducts, promoting the normal flow of bile and preventing obstructions that could lead to jaundice. Although direct evidence for this mechanism in the context of adult jaundice is scarce, its potential role in overall biliary tract function warrants further investigation.
Recommendations and Considerations for Adults with Jaundice
1. Consultation with Healthcare Providers
Given the current state of knowledge, adults with jaundice should not self-medicate with vitamin D supplements without first consulting their healthcare providers. A thorough evaluation of the underlying cause of jaundice is essential, as different causes may require different treatment approaches. A doctor can assess the patient’s vitamin D status through blood tests and determine if supplementation is appropriate, considering factors such as the patient’s diet, sunlight exposure, and any comorbidities.
2. Lifestyle and Dietary Modifications
In addition to potential vitamin D supplementation, lifestyle and dietary changes can be beneficial. For those with liver-related jaundice, reducing alcohol consumption (if applicable) and maintaining a healthy diet rich in fruits, vegetables, and whole grains can support liver function. Increasing sunlight exposure in a safe and controlled manner (while taking precautions to avoid skin damage) can also help boost vitamin D levels naturally. However, in cases where the jaundice is caused by a serious underlying condition like liver cancer or advanced cirrhosis, more aggressive medical and surgical interventions may be necessary, and vitamin D supplementation alone would not be a sufficient treatment strategy.
Conclusion
In conclusion, the relationship between vitamin D and jaund deuce in adults is complex and not yet fully understood. While in vitro and animal studies suggest potential benefits of vitamin D in modulating bilirubin metabolism and reducing jaundice severity, human clinical trials have yielded mixed results. More research, particularly large-scale RCTs, is needed to definitively establish whether vitamin D can be an effective adjunct treatment for adult jaundice. In the meantime, adults with jaundice should work closely with their healthcare providers to address the underlying cause of their condition, consider appropriate lifestyle modifications, and make informed decisions about vitamin D supplementation based on individual circumstances. By taking a comprehensive approach, we can better manage jaundice in adults and improve their overall quality of life.
Related Topics: