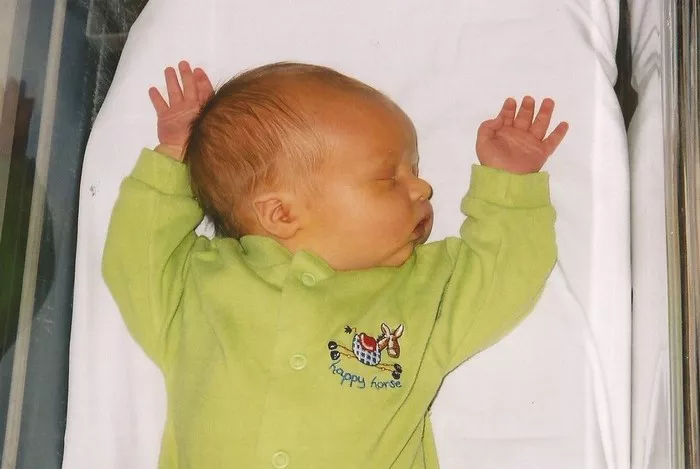
Newborn jaundice, characterized by the yellowing of a baby’s skin and eyes, is a common condition that many parents encounter within the first few days of their infant’s life. While the sight of a jaundiced newborn can be alarming, it’s important to understand that jaundice is often a normal part of the postnatal period. This article delves into the intricacies of newborn jaundice, exploring its causes, symptoms, potential complications, and treatments.
What is Newborn Jaundice?
Jaundice in newborns occurs when there is an excess of bilirubin in the blood. Bilirubin is a yellow pigment produced during the normal breakdown of red blood cells. In adults, the liver processes bilirubin and excretes it through the intestines. However, in newborns, particularly those born prematurely, the liver is often not mature enough to handle bilirubin efficiently, leading to its buildup in the blood.
Why is Newborn Jaundice Common?
Newborn jaundice is quite common, affecting approximately 60% of full-term infants and 80% of preterm infants in their first week of life. Several factors contribute to this high prevalence:
1. Increased Red Blood Cells: Newborns have a higher turnover of red blood cells compared to adults, resulting in more bilirubin production.
2. Immature Liver Function: The newborn liver is often not fully developed, which hampers its ability to process and eliminate bilirubin.
3. Reabsorption of Bilirubin: Newborns’ intestines can reabsorb bilirubin into the bloodstream before it is excreted, a process known as enterohepatic circulation.
Types of Newborn Jaundice
Newborn jaundice can be classified into several types based on its underlying causes:
1. Physiological Jaundice: The most common type, occurring due to the natural immaturity of the newborn’s liver and its inability to process bilirubin efficiently. It typically appears on the second or third day of life and resolves within two weeks.
2. Breastfeeding Jaundice: This occurs in breastfed babies in the first week of life, often due to insufficient intake of breast milk, leading to dehydration and reduced bilirubin excretion.
3. Breast Milk Jaundice: Appearing after the first week of life, this type is linked to substances in breast milk that can increase bilirubin levels. It usually peaks at two to three weeks and can last a month or more but is generally harmless.
4. Pathological Jaundice: Less common and more serious, it occurs when there is an underlying health issue, such as blood group incompatibility, infections, or enzyme deficiencies, leading to excessive bilirubin production or decreased bilirubin clearance.
Symptoms of Newborn Jaundice
The primary symptom of jaundice is the yellowing of the skin and the whites of the eyes. This discoloration typically starts on the face and spreads downward to the chest, abdomen, legs, and soles of the feet as bilirubin levels increase. Other symptoms that may accompany jaundice include:
- Poor feeding or sucking
- Lethargy or sleepiness
- Dark, yellow urine (normal newborn urine is light in color)
- Pale or clay-colored stools (normal newborn stools are yellow or orange)
Diagnosing Newborn Jaundice
Diagnosis of jaundice begins with a physical examination. Pediatricians often use a bilirubinometer, a device that measures bilirubin levels in the skin. If jaundice is suspected to be more severe, a blood test (serum bilirubin level) is conducted to determine the exact amount of bilirubin in the blood.
When is Newborn Jaundice a Concern?
While most cases of newborn jaundice are benign and resolve on their own, certain scenarios require medical attention:
1. Early Onset: Jaundice that appears within the first 24 hours of life is often more severe and warrants immediate evaluation.
2. High Bilirubin Levels: If bilirubin levels rise too high, there is a risk of bilirubin passing into the brain tissue, leading to a condition called kernicterus, which can cause permanent brain damage.
3. Persistent Jaundice: Jaundice that lasts more than two to three weeks may indicate an underlying health issue that needs to be addressed.
4. Associated Symptoms: If jaundice is accompanied by other symptoms such as fever, poor feeding, or excessive sleepiness, it’s essential to seek medical advice promptly.
Treatment Options for Newborn Jaundice
Treatment for jaundice depends on the severity of the condition and the underlying cause. For mild cases, no treatment may be necessary other than regular monitoring. For more severe cases, treatment options include:
1. Phototherapy: The most common treatment, where the baby is placed under special blue spectrum lights. The light helps break down bilirubin in the skin, making it easier for the baby’s body to eliminate it.
2. Exchange Transfusion: In cases of very high bilirubin levels, an exchange transfusion might be necessary. This procedure involves gradually removing the baby’s blood and replacing it with donor blood to quickly lower bilirubin levels.
3. Intravenous Immunoglobulin (IVIg): For jaundice caused by blood group incompatibility, IVIg can reduce bilirubin levels by decreasing the breakdown of red blood cells.
4. Treating Underlying Causes: If jaundice is due to an infection, enzyme deficiency, or another medical condition, treating the underlying issue is crucial for resolving the jaundice.
Preventing Newborn Jaundice
While not all cases of jaundice can be prevented, certain measures can reduce the risk:
1. Adequate Feeding: Ensuring that the baby is well-fed can help lower the risk of jaundice. Frequent feeding promotes regular bowel movements, which aids in the excretion of bilirubin.
2. Monitoring: Babies should be monitored for signs of jaundice, especially during the first few days after birth. Early detection can prevent severe complications.
3. Recognizing Risk Factors: Babies born prematurely, those with a family history of jaundice, or those with bruising at birth are at higher risk and should be monitored closely.
The Role of Breastfeeding in Jaundice
Breastfeeding plays a significant role in the management and prevention of jaundice. While breastfeeding jaundice can occur due to insufficient intake, it’s essential to continue breastfeeding rather than switch to formula, as breast milk provides optimal nutrition and immune support. Lactation consultants can assist mothers in ensuring their baby is feeding effectively.
Long-term Outlook for Babies with Jaundice
Most newborns with jaundice recover completely without any lasting effects. With proper monitoring and timely treatment, even more severe cases can be managed effectively. However, it’s crucial for parents to be aware of the signs of jaundice and seek medical advice when necessary.
Conclusion
Newborn jaundice is a common and usually benign condition that results from the immature liver’s inability to process bilirubin efficiently. Understanding the causes, types, symptoms, and treatments of jaundice can help parents manage this condition effectively. With vigilant monitoring and appropriate medical care, most cases of newborn jaundice resolve without complications, ensuring a healthy start for the baby.